Think before you start!
Before you even start preparing your samples, you should think about the choice of microscope for image acquisition. Manufacturers offer an ever increasing range of light microscopes- some of which may already be available in your research institutes. To help you get the best out of your imaging experiment by making the right choice of microscope, this article will highlight the main features of the different, basic light microscopes and give some recommendations (and next week we look at different confocal systems). Combination of complementary types of microscopes often helps to answer more complex experimental questions, e.g. studying the high resolution 3-D morphology of a particular cell type by confocal microscopy as well as measuring quick cellular events such as 2-D timelapse images on a high-end widefield microscope in the same experimental system. The most crucial thing is that you fully understand what a given system can deliver and more importantly what it cannot achieve. Therefore, knowledge of the general technologies and the hardware available is an essential part of your imaging expertise and experimental plan.
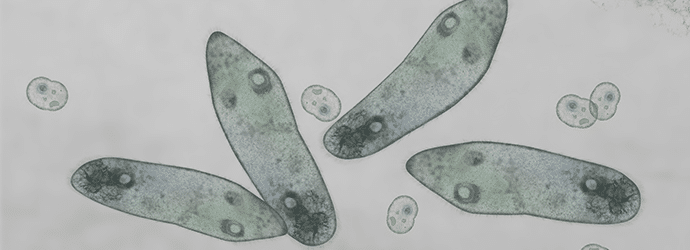
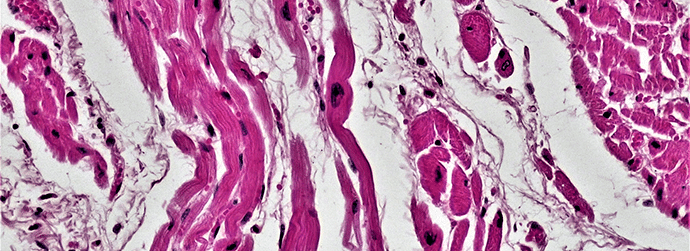
Standard light microscope – These are the basic systems for every-day use, mainly in the area of medical and histology imaging. For image acquisition, these microscopes are typically fitted with RGB cameras to acquire colour images using brightfield illumination. They are often enhanced by methods to increase the contrast in samples, such as phase contrast, differential interference contrast, and darkfield illumination. These instruments are inexpensive to run, easy to handle and provide good 2-D images of samples which have been stained with histology or immunohistological dyes. They can be equipped with software for time-lapse imaging- useful for simple live cell experiments such as cell migration assays of unlabelled cells.
Pros: Relatively inexpensive to buy and run. Robust and easy to use.
Cons: These are the basic systems. Good for 2-D imaging and simple live cell work only.
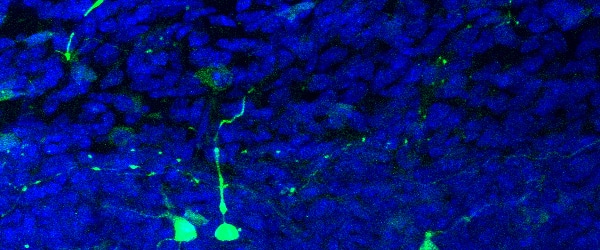
To increase labelling-specificity and image contrast, fluorescent labels (‘fluorophores’) have been introduced for biological imaging. The following light microscopy (LM) systems are all for the use with fluorescence.
Fluorescence widefield microscope – Add a bright light source for fluorophore excitation (such as a mercury or a mixed gas xenon lamp) and the right filters to a standard system and, hey presto!- you have a fluorescence widefield microscope, also referred to as epifluorescence or reflective microscope. These systems typically use cameras (CCD, EMCCD, CMOS) as detectors, which is a fast and efficient way of image acquisition. They are particularly suited for imaging fast biological events in live specimens such as quick changes of ion concentrations or fast moving cell organelles. Acquisition speed is mainly limited by the read-out speed of the camera and can be in the range of tens of milliseconds. It should be mentioned that the axial resolution (resolution in the Z-direction providing the third dimension) of these microscopes is pretty poor and out-of-focus information in the image degrades its quality. This can be corrected by image restoration, but requires the acquisition of 3-D images by recording a series of images with incrementally and precisely changing focus. Since these systems are based on combinations of spectral filters, there are limitations for multi-channel imaging beyond three fluorophores and you need to make sure that you have the right filter set available.
Pros: Easy to handle, cost-efficient, provide good lateral resolution, fast image acquisition, high quantum efficiency (depending on the camera quality). Moderate energy used, which is desirable for live specimens.
Cons: Can suffer from image degradation by out-of-focus light without image restoration. Provides poor axial (Z) resolution.
We will continue this introduction to light microscopes next week when we look at the various confocal systems on offer.